🌜 The Night We Put Sleep in a Bottle (1903) — And Why “Skills” Are Back 💤
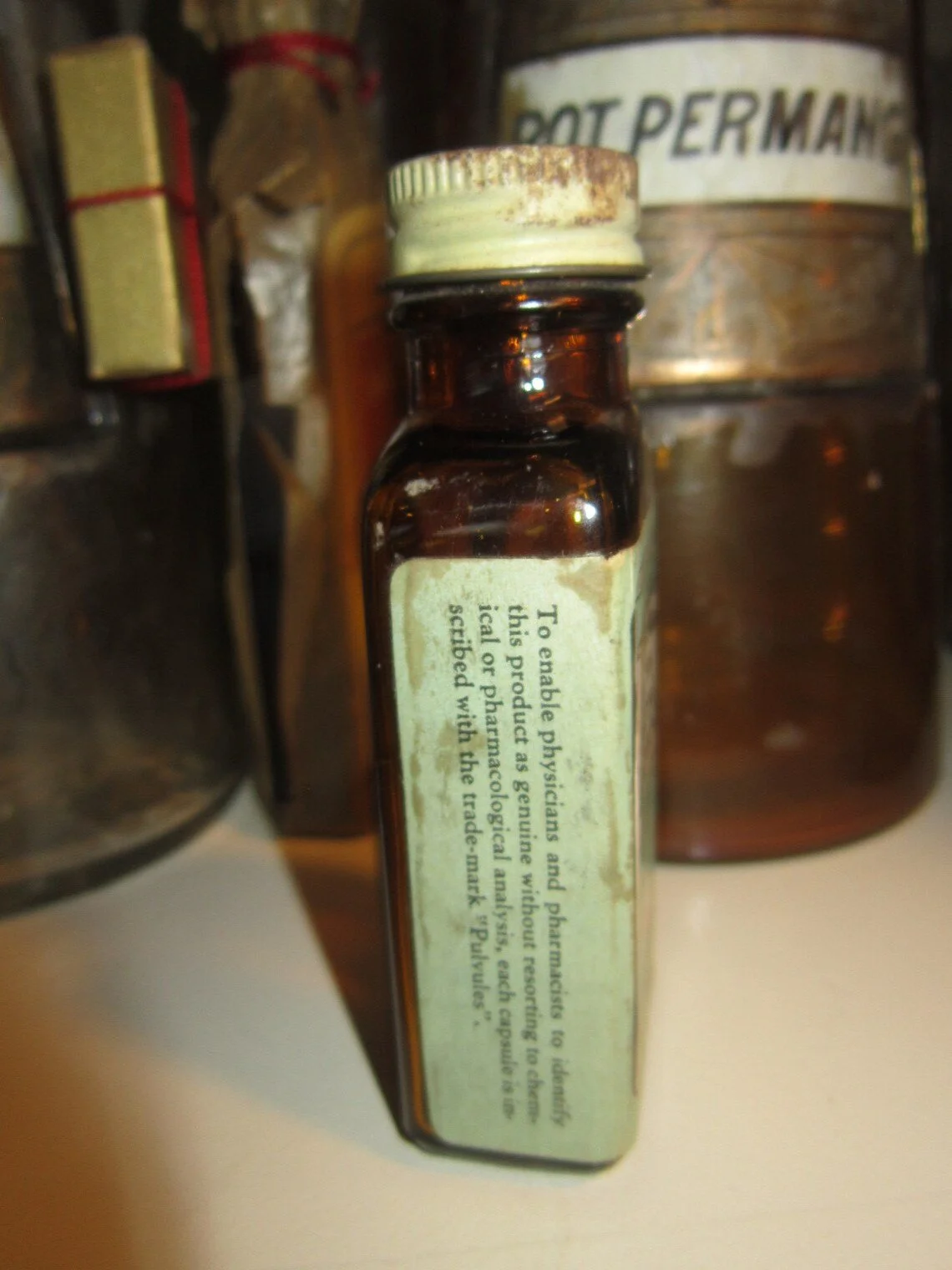
Vintage apothecary bottles, early 20th century
TL;DR: The first true prescription sleeper, barbital (Veronal, 1903), and later phenobarbital (1912) could flip the lights off—but at a cost (tolerance, overdose risk). Mid-century benzodiazepines promised safer sedation, then brought their own baggage (dependence, withdrawal, cognitive fog). The modern pivot: skills over pills for chronic insomnia (think CBT-I), plus a steady sound bed (pink/brown noise, rain, surf) to smooth disruptions so real sleep can do its repair work.
The “Off Switch” Era
In 1903, **barbital—marketed as Veronal—**arrived as the turn-of-the-century answer to modern overstimulation. A decade later came phenobarbital: longer-acting, widely used, a staple in the doctor’s black bag. For a while, the night obeyed.
Then the bill came due. Barbiturates could be brilliant—or brutal. Tolerance crept up, doses followed, and the margin of safety was thin. By mid-century, medicine reached for a new lever: benzodiazepines (starting with chlordiazepoxide/Librium). The promise: easier dosing and a wider safety window. Relief! Until familiar patterns surfaced—dependence, withdrawal, next-day fog.
Key lesson: Many drugs can switch consciousness off. Fewer build healthy sleep.
Bottle of early sedative / barbiturate medicine
Sedation ≠ Sleep
You can hush a noisy cortex without feeding the sleep architecture that matters—slow-wave sleep for tissue repair and memory consolidation, REM for emotional processing. Barbiturates and benzos can dim the lights; they don’t necessarily rebuild the house.
Ask of any sleep aid:
What system does it act on? (sedation vs. architecture support)
What happens to my sleep next week—without it?
The Pivot: Skills Over Pills
For chronic insomnia, first-line care has shifted to CBT-I (Cognitive Behavioral Therapy for Insomnia)—practical training that helps your brain relearn sleep without a chemical shove.
Core moves you can start now:
Anchor wake time. Same time daily (yes, even after a rough night). Your wake time sets tonight’s sleep pressure.
Tighten the window. Go to bed only when sleepy; get up if awake >20–30 minutes. Re-associate bed = sleep.
Tame pre-sleep worry. Schedule a 10-minute “download” earlier in the evening; write the next tiny action for each worry.
Light hygiene. Morning daylight within an hour of waking; dim, indirect light 90 minutes before bed.
Caffeine & alcohol timing. Caffeine cutoff 8–10 hours before bed; alcohol disrupts the second half of the night.
Environment. Cool (≈60–67°F / 15–19°C), dark, and predictably quiet.
Advertisement for Belbarb sedative / hypnotic
Why Sound Helps (Without Drugging the Nervous System)
Your sleeping brain is still on sentry duty. Sudden spikes (traffic bursts, hallway doors, notification pings) can trigger micro-arousals that shred continuity. A steady, broadband bed—pink/brown noise, soft rain, distant surf—masks spikesand whispers “safe” to your threat detectors.
How to set it up:
Choose the profile: Pink or brown noise for a gentle, low-end emphasis; rain/surf if you prefer nature-anchored cues.
Volume rule: Faintest effective level—enough to blur, never to blast.
Consistency: Let it run all night rather than on a timer to avoid abrupt offsets.
No plot twists: Avoid music with vocals or dynamic swings; steady > stimulating.
Tonight’s Starter Plan (15 minutes, tops)
Pick a lane: Commit to one week of “skills first.” Protect your wake time like a paycheck.
Re-tune the room: Start a pink/brown noise track at a low, steady volume.
Dim & wind down: 90 minutes pre-bed, lower lights; do a boring, repeatable ritual (wash face → stretch → paper pages or calming audio).
If you’re awake in bed: Up, dim light, quiet activity. Return only when sleepy. Train the association.
Where Medication Fits
Medication can be useful—short-term, targeted, and clinician-supervised (e.g., during acute stress or while you begin CBT-I). The long arc from 1903 to today suggests something hopeful: your brain can relearn sleep, and smart sound can help keep the pathway clear.
Safety note: If you experience loud snoring, witnessed apneas, gasping, or daytime sleepiness that affects safety, speak with a qualified clinician to rule out conditions like sleep apnea or restless legs before overhauling your routine.
Keep It Simple, Keep It Steady
Sleep rewards consistency more than heroics. Trade the nightly “hack hunt” for a few durable levers—timed light, anchored wake, gentle sound—and let biology do what it’s been designed to do.
#SleepHealth #CBTI #SleepHygiene #InsomniaHelp #RestorativeSleep #CircadianRhythm #PinkNoise #BrownNoise #NatureSounds #SoundSleep #SleepScience #Wellbeing #HealthyHabits #BetterSleepTonight #Parenting #OpioidHistory #Benzodiazepines #Barbiturates #ModernSleep #SkillsOverPills